The simple truth about cosmetic complications
Dermatologists share insight and instruction for approaching procedural afflictions, including what the specialty can do to collectively restore confidence and protect patients.

It goes without saying that dermatologists do everything in their power to keep their patients safe and avoid complications or adverse events. However, stay in the business long enough and they’re bound to occur in some form or fashion, said Michael H. Gold, MD, FAAD.
This is particularly true in the contemporary realm of aesthetic procedures, which have become exponentially desirable. Worldwide, the United States performs the highest number of cosmetic operations, with Brazil ranked a close second. Unfortunately, at the forefront of this growth is increased concern for efficiency and efficacy.
“We are witnessing both remarkable advancements and, at the same time, a growing number of complications — some of which have very serious, even fatal, consequences,” said Marcia Ramos-e-Silva, MD, PhD, IFAAD, professor and chair of dermatology at University Hospital and School of Medicine of the Federal University of Rio de Janeiro, Brazil.
Preparation is imperative, but it’s not enough to neutralize negative results. Dermatologists must possess the correct tools to identify and treat complications, particularly severe ones such as allergic reactions, disfigurement, blindness, or embolism, as soon as possible regardless of the procedural tool or root cause.
“You need to know how to fix it as soon as possible to minimize potential sequelae,” said Dr. Gold, who is medical director of Gold Skin Care Center in Nashville.
Lay the foundation and build upon it
 Dóris Hexsel, MD, IFAAD
Dóris Hexsel, MD, IFAAD
“To prevent complications, proper and continuous training is paramount. This includes staying current with new procedures, products, and equipment, as well as having a strong foundation in facial anatomy and risk areas,” said Dóris Hexsel, MD, IFAAD, dermatologist and principal investigator of Hexsel Dermatologic Clinics in Rio de Janeiro and Porto Alegre, Brazil. “Constant practice and the refinement of skills are essential to ensuring both the safety and success of treatments.”
Advancements certainly contribute to the need for ongoing training, Dr. Gold said, especially because innovations in technology can be an ally — both in terms of prevention and correction.
“For instance, lasers and light sources are much more sophisticated now compared to when they first came out, and the default settings today are much better than they used to be, which can minimize potential adverse events,” he said. “With the advent of AI, we hope that better patient selection and determination of proper procedures will also help eliminate more potential adverse events in the future.”
Dr. Hexsel urges clinicians to acknowledge risks and solutions for each procedural type and complete a thorough pre-evaluation with the patient. Assessments should consider an individual’s medical history, prior treatments, allergies, and comorbidities, she said.
“All these measures aim to approach cosmetic treatments with the seriousness they deserve, addressing each patient’s needs without excess,” said Dr. Hexsel.
 Michael H. Gold, MD, FAAD
Michael H. Gold, MD, FAAD
“Under-promise and over-deliver is something that I have always preached,” Dr. Gold said. “If I am treating melasma, I never promise a cure. If I am treating acne scars, I never promise 100% of them will be gone after our procedures.”
Once all the preoperative actions are complete, there should be a constant feedback loop to assess throughout the process and be able to spot any adverse events. That goes for the physician and the patient.
“Continuous follow-up after the procedure is necessary,” Dr. Hexsel said. “Doctors should remain available to monitor the treatment’s progress and identify any complications early. If any unexpected symptoms arise, patients should be instructed to contact the doctor immediately.”
Keep calm and intervene
A leading cause for concern, particularly in Brazil, is the astonishing amount of cosmetic procedures performed by underqualified individuals, said Dr. Ramos-e-Silva. Other clinicians, like dentists, therapists, or nurses, as well as nonmedical specialists with minimal to no training are touting themselves as qualified, when it should be board-certified dermatologists or cosmetic/plastic surgeons completing the work.
 Marcia Ramos-e-Silva, MD, PhD, IFAAD
Marcia Ramos-e-Silva, MD, PhD, IFAAD
As the qualified professionals, she said, dermatologists must understand the breadth of contraindications, challenges, and potential complications. She also recommends establishing well-defined emergency protocols.
“We are often the ones who must diagnose and treat complications, whether in our own patients or in those referred to us. No one is immune to encountering these challenges,” she said. “Even when procedures are performed with the highest level of expertise, complications can still arise. The key is knowing how to prevent, recognize, and effectively manage them from the beginning.”
Know the work, do the work
Dr. Ramos-e-Silva, along with numerous experienced colleagues, are part of the Brazilian Study Group on Dermatologic Procedures and Complications. The consortium collaborates on case analyses, shared solutions, and improved safety measures, and it has published scientific articles and presented symposiums.
“My hope is to instill greater confidence and less fear in dealing with these complications. Rather than seeing them as obstacles, we must view them as opportunities to improve patient care and safety,” Dr. Ramos-e-Silva said. “With proper knowledge and preparation, we can ensure that these procedures — when done correctly — remain the powerful, quality-of-life and self-esteem-enhancing treatments they are meant to be.”
Below, experts from the group provide input on leading practices and techniques with recommendations on how to mitigate, manage, or correct complications.
Aesthetic procedures
 Gisele Viana Oliveira, MD, MSc, PhD, IFAAD
Gisele Viana Oliveira, MD, MSc, PhD, IFAAD
In Brazil, where she is a practicing dermatologist and professor at Medical Sciences School of Minas Gerais, Dr. Viana Oliveira said the influx in scarring is partially due to unlicensed professionals practicing these cosmetic methods in inadequate settings using deficient tools or training. When these operations go wrong or create unnecessary complications, the patients come to her for rectifications.
 Natural results (right) obtained after treating hypertrophic scars on a burned patient using the ASAP nonsurgical sequential algorithm.doi:10.1111/jocd.13792
Natural results (right) obtained after treating hypertrophic scars on a burned patient using the ASAP nonsurgical sequential algorithm.doi:10.1111/jocd.13792
- Assess, or analyze, the injury prior to treatment.
- Soften the scarred area before injections, using occlusive silicone or hydrocolloid dressings.
- Approach therapy with proven injections and laser technologies.
- Address pigmentation and quality of the skin once the scar is flat.
Following these four stages may take nine months to a year to complete, depending on severity of the lesion(s), Dr. Viana Oliveira said, but will produce the best and longest-lasting results.
Chemical peels
 Carlos G. Wambier, MD, IFAAD
Carlos G. Wambier, MD, IFAAD
For several years, dermatologists and pharmacists have been evaluating noncardiotoxic chemicals, such as trichloroacetic acid (TCA) and glycolic acid (GA), as alternatives to phenol for delivering phorbol esters found in croton oil.
“TCA 35% creates a ‘TCA-croton oil’ chemical peel, which seems to cause more rejuvenation than the traditional medium depth peels,” said Dr. Wambier, who is associate professor of dermatology at Brown University and vice president of the International Peeling Society (IPS).
Dr. Wambier said qualified, board-certified dermatologists need to take control of performing such procedures and utilizing these drugs through requisite advocacy efforts.
“The AAD and the IPS should help agencies achieve appropriate regulations,” he said.
Ultrasound-guided therapy
 Fernanda Cavallieri, MD
Fernanda Cavallieri, MD
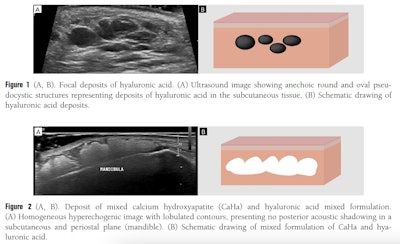
“Using high-frequency ultrasound as a first-line imaging technique offers real-time visualization of each skin layer,” she wrote in a 2023 study, “Ultrasound in Aesthetics.”
Dr. Cavallieri is the medical director at Clínica Cavallieri and serves as vice chair of the Dermatology Community at the American Institute of Ultrasound in Medicine. She also co-founded a complications diagnosis & management course, which instructs clinicians on how to implement ultrasound-guided procedural methodology.
“As the demand for injectables and other aesthetic treatments increases, so does the incidence of complications such as vascular occlusions, nodules, abscesses, and panniculitis,” she said. “Identification of different types of fillers helps professionals make safer clinical decisions, guide hyaluronidase injections, and distinguish between different types of complications. This ultimately leads to more effective treatments, reduced risks, and better patient outcomes.”
 Gabriela Helena Munhoz da Fontoura, MD
Gabriela Helena Munhoz da Fontoura, MD
Bruising can be a distressing result of biostimulators, though it is typically temporary and nonthreatening, said Dr. Munhoz. She recommends patients manage the treated area with cold compresses, gentle massage, and arnica cream or topical vitamin K. For extensive or persistent bruising, clinicians can apply low-energy intense pulsed light once daily until resolved.
Allergic reactions to biostimulator injections can be troublesome and dermatologists should monitor patients for any negative responses, especially anaphylaxis, she said.
Another difficult but conceivable complication is a bacterial infection, said Dr. Munhoz.
“Infections should be suspected when the patient initially presents with a nodule or multiple nodules at the injection site, where the biostimulator was administered,” she said. “At this point, an ultrasound should be requested, as it will likely reveal a fluid collection. It is essential to obtain a sample for microbiological analysis in order to identify the responsible pathogen or bacterial agent.”
There is also the possibility of persistent edema or persistent intermittent delayed swelling (PIDS), both of which can occur weeks or months after the procedure, Dr. Munhoz said. Edema can be treated with a three- to five-day period of 40 mg steroids. PIDS, an immune-triggered response, can be confirmed with ultrasound and treated with a week-long oral steroid and/or antihistamine.
Other known complications of biostimulator therapy include:
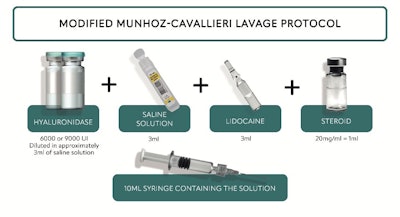
- Sterile abscesses, which should be managed using the Munhoz-Cavallieri Lavage Protocol.
- Delayed onset nodules, for which biopsies often reveal a foreign body reaction and/or fibrosis.
- Vascular events, which are most associated with hyaluronic acid fillers.
“Clinicians should be vigilant when a patient reports pain, livedo reticularis, or any signs of cutaneous hypoperfusion within hours after a biostimulator injection,” Dr. Munhoz said. “We recommend that treatment should include oral corticosteroids, aspirin, and hyaluronidase until complete clinical resolution. In many cases, hyperbaric oxygen therapy is also indicated.”
 Maria Fernanda Tembra, MD, IFAAD
Maria Fernanda Tembra, MD, IFAAD
Maria Fernanda Tembra, MD, IFAAD, has witnessed the filler craze and knows that “more is not always better.” Over time, transitory fillers can produce unwanted, unnatural, and often painful results, including sterile abscesses, PIDS, vascular occlusions, and the Tyndall effect, or bluish discoloration that can directly result from filler injections.
Like her colleagues, Dr. Tembra recommends using ultrasound to confirm the type of filler and precise effect, then follow the Munhoz-Cavallieri Lavage Protocol.
“We know that there is a different range of products that may be used as dermal fillers, but only hyaluronic acid-based ones are able to dissolve with hyaluronidase. So before starting treatment, it is important to know which product has been used,” she said.
 Angioedema due to the injection of hyaluronic acid.Maria Fernanda Tembra, MD, IFAAD
Angioedema due to the injection of hyaluronic acid.Maria Fernanda Tembra, MD, IFAAD
When it comes to permanent fillers, complications can include physical deformities like inflammatory granulomas or chronic edema, as well as systemic effects like hypercalcemia and renal insufficiency, said Mayra Ianhez, MD, PhD. These can occur months to years after the initial injection and can be treatment-resistant, necessitating a novel immunomodulatory approach, she said.
“As the landscape of aesthetic medicine evolves, dermatologists must be equipped to manage not only the aesthetic outcomes but also the complex immunologic consequences of procedures once thought to be ‘low risk’,” said Dr. Ianhez, who is a dermatologist, researcher, and professor at Federal University of Goiás and Hospital of Tropical Diseases in Brazil. “My ongoing research focuses on cytokine profiling of affected tissues to develop more targeted and effective immunosuppressive treatments.”
 Top photos (a, b) portray nodules and erythema in the nasolabial fold as a result of permanent filler injections. Bottom photos (c, d) demonstrate results after treatment with JAK inhibitors.Mayra Ianhez, MD, PhD
Top photos (a, b) portray nodules and erythema in the nasolabial fold as a result of permanent filler injections. Bottom photos (c, d) demonstrate results after treatment with JAK inhibitors.Mayra Ianhez, MD, PhD
- Initiate conservative therapies, such as corticosteroids or methotrexate (MTX).
- Advance to JAK inhibitors (e.g., tofacitinib, upadacitinib, or abrocitinib) which have shown increasingly positive results for patients experiencing chronic or severe adverse events.
- Perform surgery only as a last resort.
“These findings support a paradigm shift — moving away from surgical excision and long-term corticosteroid use toward precision immunotherapy,” Dr. Ianhez said.