AAD/NPF Guidelines: Managing psoriasis
Session explored four areas of psoriasis management.
Psoriasis isn’t just a skin condition. It’s a systemic immune-mediated disease that can impact a patients’ quality of life and their risk of comorbidities. To improve patient care, Friday’s S001 – AAD/NPF Guidelines focused on four important areas of psoriasis management.
Reclassifying psoriasis severity
To categorize psoriasis severity and prescribe the most appropriate treatment, dermatologists often rely on body surface area to calculate a psoriasis area and severity index (PASI) score. But body surface area can be a poor indicator of psoriasis severity in patients with special site involvement.
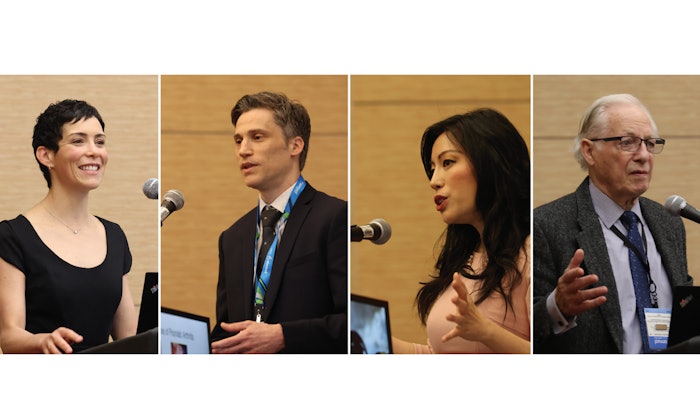
“Special areas are commonly involved in psoriasis patients, including the scalp, palms, soles, nails, and genitals, which can create more burden in terms of quality of life and psychosocial issues,” said Mary E. Horner, MD, FAAD, with Dermatology Consultants of Sacramento, California. “If you have a patient with body surface area of 1%, but it’s on your palms, it’s going to be painful. If it’s on your face, how might that affect your relationships and your career choices?” Dr. Horner presented evidence that quality of life — the Dermatology Life Quality Index — may be a better indicator of psoriasis severity. Traditional definitions of moderate and severe psoriasis, based on body surface area, are inadequate to determine the need for systemic/biologic therapy, Dr. Horner said. Special areas of involvement should upgrade severity irrespective of body surface area involvement. “Adhering to BSA rules creates undertreatment, based on true patient needs,” Dr. Horner said. “We need to ask our patients: ‘How is your psoriasis affecting your life?’”
Detecting psoriatic arthritis earlier
About 30% of patients with psoriasis will develop psoriatic arthritis. Psoriasis usually precedes the onset of psoriatic arthritis by an average of five to 10 years in approximately 80% of patients. “There are ways we can help our patients early on in the game,” said Dario Kivelevitch, MD, FAAD, dermatology residency program director, Baylor Scott & White Health in Dallas. To identify psoriatic arthritis, Dr. Kivelevitch employs the Psoriasis Epidemiology Screening Tool, which asks patients five questions. “Early detection and treatment can prevent joint destruction. Dermatologists should screen psoriasis patients for psoriatic arthritis at every visit,” Dr. Kivelevitch said. He presented treatment options based on the 2018 ACR/NPF Guidelines for the Treatment of Psoriatic Arthritis, of which only 6% are strong recommendations. “We need more evidence to develop guidelines for better management,” he said.
Comparing biologic medication
Which biologic drug is the best option for your psoriasis patient? Network meta-analysis can help you decide, said presenter April W. Armstrong, MD, MPH, FAAD, associate dean of clinical research at the Keck School of Medicine at the University of Southern California in Los Angeles. Network meta-analyses compare multiple treatments simultaneously in a single analysis, combine direct and indirect evidence, and assess the comparative effectiveness of different treatments. Dr. Armstrong discussed the utility of network meta-analysis for comparing the efficacy and safety of the 11 FDA-approved biologic medication for psoriasis, using selected published network meta-analysis in psoriasis since 2020. When evaluating the results, it’s important to ask: What outcomes are being measured and in what specific time period? Your conclusion may be different if you look at an early versus later time period, Dr. Armstrong cautioned.
Cardiovascular comorbidities
Alan Menter, MD, FAAD, a leader in guidelines development and our understanding of psoriasis and psoriatic arthritis, wrapped up the session with a discussion of the relationship between psoriasis and cardiovascular comorbidities.
“Psoriasis is not a skin disease. It’s a systemic immune-mediating disease, and systemic inflammation is critical. Systemic inflammation is also part of cardiovascular disease.” Dr. Menter urged dermatologists to screen for cardiovascular risk factors in their patients with psoriasis and manage them according to national guidelines.
