What’s new in early-stage melanoma?
New session reveals the latest information.
F020 – The Changing Landscape of Early-Stage Melanoma Management
Friday, March 25 | 1 – 3 p.m.
Room: 258C
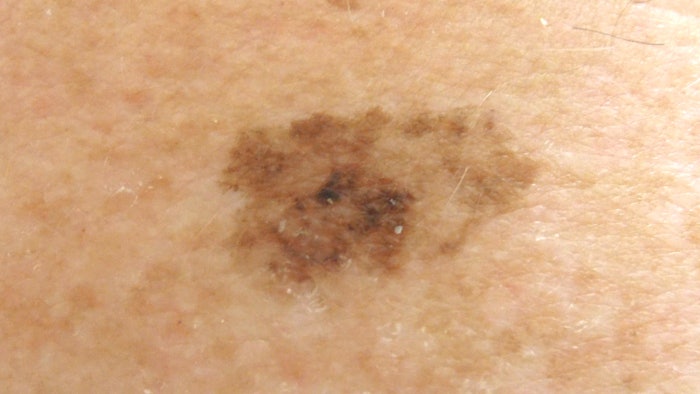
Management of early-stage melanoma (melanoma confined only to the skin) continues to evolve. Changes and advances in diagnostic techniques and tools are changing the way we think about prevention strategies and treatment plans.
“Melanoma is a condition that comes up every day in a general dermatology practice,” said Michael E. Ming, MD, FAAD, associate professor of dermatology at the University of Pennsylvania Perelman School of Medicine in Philadelphia. “Recent changes in the field could affect how we think about early-stage melanoma and how we discuss it with our patients.”
Dr. Ming will chair the new forum, F020 - The Changing Landscape of Early-Stage Melanoma Management. Attendees can expect the latest on issues such as how to choose appropriate genetic testing for melanoma patients or their relatives, considerations when counseling patients about the use of sunscreens, the role of gene expression profiling, surgical treatment options, and the availability of clinical trials.
Genetic expression profiling at the bedside and improved imaging technology is already moving out of academic centers into dermatology practices nationwide.
Sorting out latest sunscreen data
Today’s session will also address some of the current controversies surrounding the use of sunscreen. Some jurisdictions have banned the use of certain common sunscreen ingredients, due to the possibility that they could affect marine life studies. It also has raised the question of potential harm to human users from some ingredients.
“An estimated 14,000 tons of sunscreen washes off humans into the oceans every year,” Dr. Ming said. “We will be exploring the data to see whether that poses a theoretical risk to marine life or if there is concrete evidence of harm. And we will discuss the current literature and how to counsel patients about whether there is demonstrable harm to themselves if they use specific ingredients, or if that risk is only theoretical.”
New tests and technologies
“As dermatologists, we welcome new technologies to help us diagnose melanoma,” said Caroline C. Kim, MD, FAAD, director of the Melanoma and Pigmented Lesion Programs at Tufts department of dermatology. “However, it is important to understand strengths and limitations of these new tests and technologies as well as potential utilization strategies to best serve our patients. Adhesive genetic expression profiling tests, for example, are a currently available, non-invasive testing option for concerning pigmented lesions. Updated imaging technology can have a similar impact on practice.”
For many physicians and patients, it can be challenging to keep up with new developments. “There are more options in technology now to assess genetic variation related to patients’ cancers. It can be a little confusing to figure out which test (if any) is more appropriate for which patient at a given time,” said Emily Y. Chu, MD, PhD, FAAD, associate professor of dermatology at the University of Pennsylvania.
New molecular testing being employed
Somatic molecular testing is being used to help guide therapeutic decisions in more advanced melanoma, Dr. Chu said. For early-stage disease, molecular tests have been developed that may help distinguish between melanoma and benign lesions that can mimic cutaneous melanoma under the microscope. And growing numbers of patients arrive at appointments with “information” collected online that may — or may not — be relevant or even accurate.
“Having as much valid information as possible is incredibly helpful from the clinician standpoint when you are taking care of patients who are increasingly savvy but may not have all of the information or the context to put it into perspective,” Dr. Chu said. “As physicians, we have to be aware of the current genetic and molecular testing options.”
The literature is complicated when discussing the value of molecular testing in early-stage disease. The debate is often framed in yes/no statements, but the practical value is more nuanced.
“Key controversies in early-stage melanoma management include utilization of molecular techniques that can aid in melanoma diagnosis and prognosis, particularly various gene expression profiling (GEP) tests,” said Susan Swetter, MD, FAAD, professor of dermatology and director of the Pigmented Lesion and Melanoma Program at the Stanford University Medical Center in Stanford, California. “GEP tests may serve an adjunctive role to melanoma stage and other clinopathologic factors that help predict outcome or likelihood of sentinel lymph node biopsy, but they are not yet incorporated into national melanoma guidelines as part of routine care. This session will help explain the current state of molecular testing for melanoma diagnosis and management.”
Melanoma and surgery
There are also controversies surrounding surgical approaches to early-stage melanoma. Mohs micrographic surgery and staged excision with permanent sections have been reported as more effective in reducing local recurrence in certain melanoma subtypes, mainly melanomas in situ and thin invasive melanomas in chronically sun-exposed areas of the head or on acral sites, which are anatomically constrained. However, prospective data for Mohs surgery or staged excision with permanent sections versus conventional wide excision are lacking when it comes to thicker invasive melanomas.
More emphasis on evidence-based recommendations
“Dermatologists ‘own’ the field of early melanoma and should be thoroughly up-to-date on current evidence-based recommendations,” Dr. Swetter said.
Up-to-date includes the latest drug approvals, including pembrolizumab, which the FDA okayed for Stage II B and C melanoma in late 2021.
“This is a very positive change for patients who are sentinel lymph node negative, but we know are still at high risk for recurrence,” explained Giorgos Karakousis, MD, associate professor of surgery at the University of Pennsylvania Perelman School of Medicine.
“At the same time, there are other neoadjuvant therapies that are still in clinical trials that will be discussed. Melanoma is one of the most lethal skin diseases out there, which makes having a good grounding in the new and innovative approaches to early-stage disease all the more important for physicians.”
Visit AAD DermWorld Meeting News Central for more articles.
