Consider the possibilities
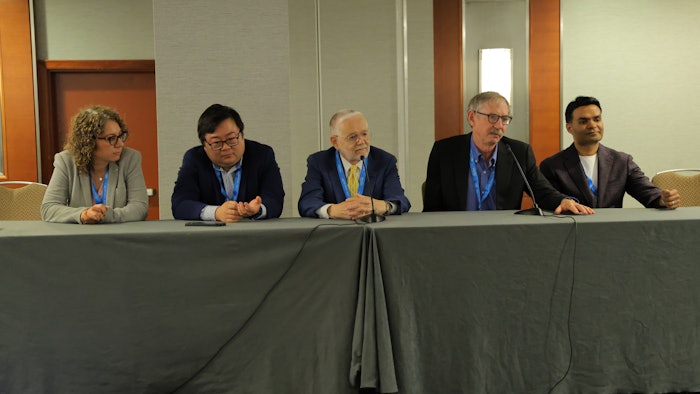
The Future of Dermatology Symposium introduced impending innovations in technology and therapy at the confluence of academia and biopharma.
Imagine a topical treatment that can prevent androgenetic alopecia (AGA) and hair graying. It seems too good to be true. Yet, it’s one of the possibilities on the horizon.
This prospect and many more were spotlighted in Thursday’s session, F001 – Future of Dermatology Symposium: The New Skin Frontier: Innovation at the Intersection of Biopharma and Academia. Jon Edelson, MD, chairman, CEO, and president of Eirion Therapeutics, Inc., was among the panelists at the session. Dr. Edelson shared his company’s successful results from its first-in-human clinical trial of ET-02, a once-daily topical treatment for AGA.
“ET-02 employs a non-hormonal mechanism of action that inhibits the molecular pathway causing hair follicle stem cells to become quiescent, reactivating them and resulting in renewed healthy hair growth,” Dr. Edelson said. “ET-02 has the potential to not only treat but prevent both AGA and hair graying.”
Willing participants
Dr. Edelson told attendees about the results of a 2024 survey reported by the Wall Street Journal. Of the 9,000 U.S. people queried, one-third said they would “probably or definitely” take a drug to prevent or reverse hair graying if such a medication were approved.
Regarding its benefits for AGA, the ET-02 clinical trial found the amount of hair growth achieved after one month of the topical’s once-daily 5% dosage was greater than the amount achieved after four months of twice-daily 5% topical minoxidil, as studied in minoxidil’s separate clinical trials.
Tech talk
Thursday’s symposium underscored the prospects of solutions dermatology, defined by the specialty’s drive to be innovators, entrepreneurs, and visionaries in the quest to serve patients.
The session provided a platform for dermatologists to share new research abstracts. Luisa Polo Silveira, MD, from Memorial Sloan Kettering Cancer Center in New York, presented a study that explored the use of artificial intelligence (AI) in analyzing cellular-resolution full-field optical coherence tomography (CRFF-OCT) images to distinguish melanomas from nevi. Using an AI-driven, computer-aided detection (CADe) system, researchers quantified melanocyte morphology and melanin distribution in 17 pigmented lesions, including malignant melanomas (MM), melanomas in situ (MIS), and nevi.
According to Dr. Polo Silveira, the AI system detected significant differences in dendritic cell characteristics, nuclear morphology, and melanin patterns across lesion types. These objective measurements highlight characteristics that could help differentiate benign from malignant lesions, potentially supporting diagnostic accuracy.
“This study is important because current methods for diagnosing pigmented skin lesions rely heavily on visual interpretation, which can be subjective and prone to variability,” Dr. Polo Silveira said. “By using AI to objectively analyze OCT images, we can identify consistent morphological features associated with malignancy. This approach could enhance diagnostic precision, reduce unnecessary biopsies, and aid in earlier detection of melanoma — ultimately improving patient outcomes and streamlining dermatologic care.”
Expanding this research in the future with larger cohorts and validating findings across diverse skin types could help integrate the technology into routine clinical practice, Dr. Polo Silveira said.
AI’s long reach
The possibilities for incorporating AI don’t stop there. Kevin Tabatabaei, a medical student at Mayo Clinic Alix School of Medicine in Jacksonville, Florida, presented research that compared the diagnostic accuracy of consumer-facing AI models on smartphone-captured dermatologic images.
With the rise of multimodal AI models, patients increasingly seek dermatologic diagnoses by uploading smartphone photos to AI chatbots, Tabatabaei said. Current dermatologic AI literature heavily explores ChatGPT but neglects competitors such as Anthropic’s Claude and Google’s Gemini models.
Tabatabaei’s research evaluated three flagship chatbot versions (GPT-4o, Claude Sonnet 3.5, and Gemini 1.5 Pro) on smartphone-style images from Google’s crowdsourced “SCIN” dataset, developed with Stanford Medicine. Results indicated GPT-4o demonstrated superior performance with 56.3% top-1 accuracy and 77.1% top-3 accuracy. Claude achieved 45.5% top-1 and 66.0% top-3 accuracy, while Gemini reached 45.7% top-1 and 69.4% top-3 accuracy.
Content moderation filters in certain models prevented complete analysis of all cases, Tabatabaei said, potentially affecting comparative performance metrics. OpenAI’s GPT-4o (the premier model currently used by ChatGPT) would refuse to do about 10% of all the cases, likely due to content restrictions, he said.
“Although AI models show promising accuracy in dermatologic diagnosis from smartphone images, significant gaps remain compared to physician diagnosis. These findings are crucial as patients increasingly seek AI-guided dermatologic advice,” said Tabatabaei. “Right now, AI isn’t as good as dermatologists in diagnosing skin conditions, but it’s not too bad either.”
Treatment transformations
 Bobby Reddy, MD
Bobby Reddy, MD
In previous decades, monoclonal antibodies transformed the treatment landscape for dermatology, especially for psoriasis and atopic dermatitis. Newer treatment modalities, including bispecific antibodies and gene therapy, represent advancements in science and technology that can further benefit patients, Dr. Reddy said.
Earlier this year, the U.S. Food and Drug Administration (FDA) approved an autologous cell-based gene therapy for adults and pediatric patients with recessive dystrophic epidermolysis bullosa (RDEB), a highly debilitating genetic skin disease.
“Prademagene zamikeracel (Zevaskyn) demonstrated remarkable efficacy in a phase 3 clinical trial for patients suffering from RDEB, leading to the approval. This product, developed by Abeona Therapeutics, is expected to be available for patients in Q3 of this year and represents a tremendous victory for RDEB patients and their families,” Dr. Reddy said.
In looking at innovative therapies and technologies emerging at the intersection of biopharma and academic research, Dr. Reddy referenced a recent study from the University of Maryland that was published in Scientific Reports. In this study, researchers developed a novel blood test using flow cytometry to identify specific immune profiles. They performed this test on a patient with erythroderma, a severe and potentially life-threatening disease, and identified pathologic elevations of cytokines (interleukin-13 and -17). Based on these findings, the patient was initiated on a dual therapy of two monoclonal antibodies, dupilumab and secukinumab. The treatment led to a decline in the pathologic elevation of cytokines and a clinical resolution of erythroderma in the patient.
“This highlights the immense value which can be created by the synergy of innovative academic research and biopharma-developed products and pipelines,” Dr. Reddy said.
Merge ahead
Lilit Garibyan, MD, PhD, FAAD, a session presenter and associate professor of dermatology at Harvard Medical School in Boston, said it’s the intersection of academia and clinical practice that represents the future of dermatology.
“This is where clinicians identify unmet needs and work collaboratively with researchers and engineers, using tools to create and test new solutions, and where industry supports this work and takes the lead in commercializing solutions created in academia,” Dr. Garibyan said. “We’re seeing dermatology leap from being a specialty focused solely on the skin to one that touches the entire body.”
 Lilit Garibyan, MD, PhD, FAAD
Lilit Garibyan, MD, PhD, FAAD
“This is about rethinking the skin as a platform for systemic care. Coupling this capability with data collected through the skin to AI and machine learning is a powerful tool that will most definitely change the way we monitor and manage systemic and chronic diseases,” Dr. Garibyan said. “As someone who’s spent my career bringing ideas from lab to life, I see dermatology and the skin as the portal to systemic insight, intervention, and innovation.”
Dr. Garibyan said she has witnessed advances in dermatology firsthand, referencing her lab’s work in developing an injectable cooling technology that began as a sterile ice slurry for selectively targeting lipid rich tissue, such as fat cells and myelin sheaths around nerves.
“That invention launched Brixton Biosciences, which is commercializing this technology as a long-lasting and non-opioid therapy for pain,” Dr. Garibyan said. “This is a company that I co-founded and is currently conducting pivotal trials for the treatment of osteoarthritis knee pain.”
Dr. Garibyan said it’s essential to bring clinicians into the innovation pipeline to advance the future of dermatology.
“Clinicians are the ones who know where the pain points are, who know where current therapies fall short, and who can guide real-world usability,” she said. “Innovation isn’t a relay race with a baton passed from academia to industry. It’s a collaborative feedback loop where each sector informs, strengthens, and accelerates the others. That’s how we go from ‘interesting idea’ to ‘available treatment’ in record time.”