Using data to make a difference
Leveraging DataDerm™, new AI tool helps detect rare disorders early and advantageously.
All doctors know that correctly diagnosing and treating health conditions as early as possible can save lives. Now, a new artificial intelligence (AI) tool takes diagnostics to the next level. Patient Finder was the focus of Friday’s Annual Meeting session, U014 – Using Artificial Intelligence for Rare Dermatologic Diseases: Getting the Right Patients the Right Treatment at the Right Time.
In the informative session, Marta J. Van Beek, MD, MPH, FAAD, shared how a group of dermatologists and data gurus collaborated to apply this groundbreaking tool to dermatologic diseases.
“I think all of medicine is trying to figure out how AI fits into our workflows,” said Dr. Van Beek, who is executive medical director at the University of Iowa Ambulatory Clinics. “Everyone wonders: Will AI be able to diagnose patient conditions, in addition to decreasing administrative burden? Will it be able to find the disease earlier in the patient’s journey to get the right treatment at the right time?”
Needle in a haystack
 Marta J. Van Beek, MD, MPH, FAAD
Marta J. Van Beek, MD, MPH, FAAD
GPP is a challenging condition to diagnose, Dr. Van Beek said, as it is frequently confused with an infection when patients are not seen by a dermatologist. Patients are very sick, presenting with painful pustules on their skin and high white blood cell counts. This is a problem if a doctor doesn’t know what GPP is or what else to consider, she said.
“They may put patients on an antibiotic and treat it as infection, but in reality, GPP needs therapy that targets the immune system,” said Dr. Van Beek.
The good news? A few years ago, the U.S. Food and Drug Administration (FDA) approved spesolimab-sbzo (Spevigo) for the treatment of GPP in adults and children over the age of 12 years. And it’s proven to be effective, Dr. Van Beek said.
The bad news? GPP and other rare dermatologic diseases remain very difficult to diagnose.
“Often in medicine, when there is no effective treatment for a disease, patients suffering from that disease don’t seek health care. We then erroneously think the disease is rare because it doesn’t get diagnosed or it is misdiagnosed,” she said. “But once we find an effective treatment, patients seek care, and we realize the disease might be more common. Now is the time to actually identify these patients earlier.”
Enter: Patient Finder.
Mind the data
With the help of reliable data sources and AI, dermatologists can employ modern resources to help accurately and proactively identify these perplexing ailments. Luckily, for Dr. Van Beek et al, they didn’t have to look far.
A decade ago, AAD launched DataDerm™ — the largest dermatologic clinical registry in the world. “DataDerm was established to make sure [dermatologists] could tell our own story about our patients, whether it’s for advocacy purposes, to find cures, or to improve patient care and outcomes,” she said.
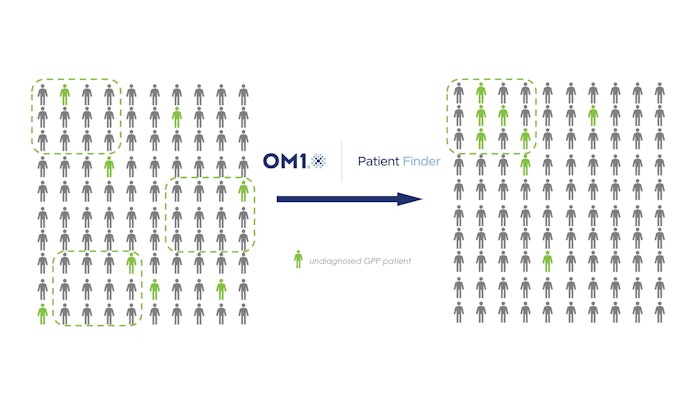
Patient Finder searches the more than 15 million patients stored in DataDerm, analyzing confirmed cases of GPP and looking for commonalities among patient populations to reveal individuals with a high probability of having or developing GPP.
Joseph Zabinski, PhD, MEM, a leader from health care technology company OM1, which developed Patient Finder, also participated in the panel. He said the AI model uses digital phenotyping to provide clues on at-risk patients who have gone undiagnosed or have been misdiagnosed and then accelerates the time to treatment.
“[Patient Finder] identifies patterns in patients’ health histories associated with target diseases, based on training on billions of datapoints,” said Dr. Zabinski, vice president and head of commercial strategy and AI at OM1. “The tool isolates phenotypic ‘fingerprints’ in the data, and we can study these fingerprints for new information about patient journeys and use them to screen others’ data.”
Why AI?
 Joseph Zabinski, PhD, MEM
Joseph Zabinski, PhD, MEM
“AI tools are growing very rapidly in maturity and clinical usefulness,” he said. “They can bring analytic clarity and personalization to the conversations patients and physicians have, including those around diagnosis and decisions around treatment plans. … [OM1 helps] demystify these tools and demonstrates how in collaboration with dermatologists, they can be tremendously helpful.”
In addition to identifying at-risk patients, Dr. Zabinski said AI tools can learn from patient records and help physicians make more informed assessments. Consider a group of patients who responded well to a certain medication and compare them to another group that didn’t respond well to the same medication. The tool can understand what each group has in common, then predict if a new patient with the same condition will or won’t benefit from the drug based on captured characteristics.
Be selective and vigilant
In this case, Patient Finder has made the nearly impossible, possible. However, AI comes with risks, said Dr. Van Beek, particularly accuracy and bias.
An AI model can generate false findings or misleading results. This occurs when the data that trains the AI tool is inaccurate, insufficient, or prejudiced. And if these biases go unnoticed or the model isn’t properly recalibrated, the hole keeps getting deeper.
For example, Dr. Van Beek said other companies have pursued tools that help with diagnoses, but their catalogs of skin images lacked diversity. This led to the technology being unable to identify lesions on patients with darker skin, and it demonstrates the criticality of selecting an AI-training source that is rich and reliable.
While DataDerm is a leading resource for the specialty, using AI still requires ongoing regulation.
“We prefer not to call it artificial intelligence, but augmented intelligence,” said Dr. Van Beek. “We don’t believe AI should be used without human oversight. It can augment what you’re doing, but it shouldn’t substitute what you’re doing. Health care is too precious.”
Looking ahead
The testing period of Patient Finder recently wrapped up, said Dr. Van Beek. So, the next steps are still being finalized. It could be used as an educational tool, she said, or it may be deployed into individual practices so physicians can employ it within their own EMR and patient base.
Dr. Zabinski shared that Patient Finder has shown success in diagnostic and therapeutic areas of several other skin conditions. In fact, fellow speaker Steven Daniel Daveluy, MD, FAAD, reviewed how Patient Finder can assist in identifying patients who may have hidradenitis suppurativa (HS).
In the end, the panelists agreed that Patient Finder is an innovative tool that can shine light on patterns in patient populations, but it is the dermatologist who has the ability — and responsibility — to confirm diagnosis and assign the correct treatment.
“That,” Dr. Van Beek said, “can be lifechanging for a patient.”
Editor’s note: The GPP project described above was generously supported by Boehringer Ingelheim. The HS project described above was generously supported by Novartis. The AAD is grateful for the support of these two important demonstrations of the power of DataDerm.











